Robert Ziltzer, MD, FACP, FAAP, FOMA
There are many choices when it comes to anti-obesity medications. The recent release of Wegovy® (Semaglutide) has been very effective leading to 15% weight loss. Let’s look at why phentermine is still the most used weight loss medication.
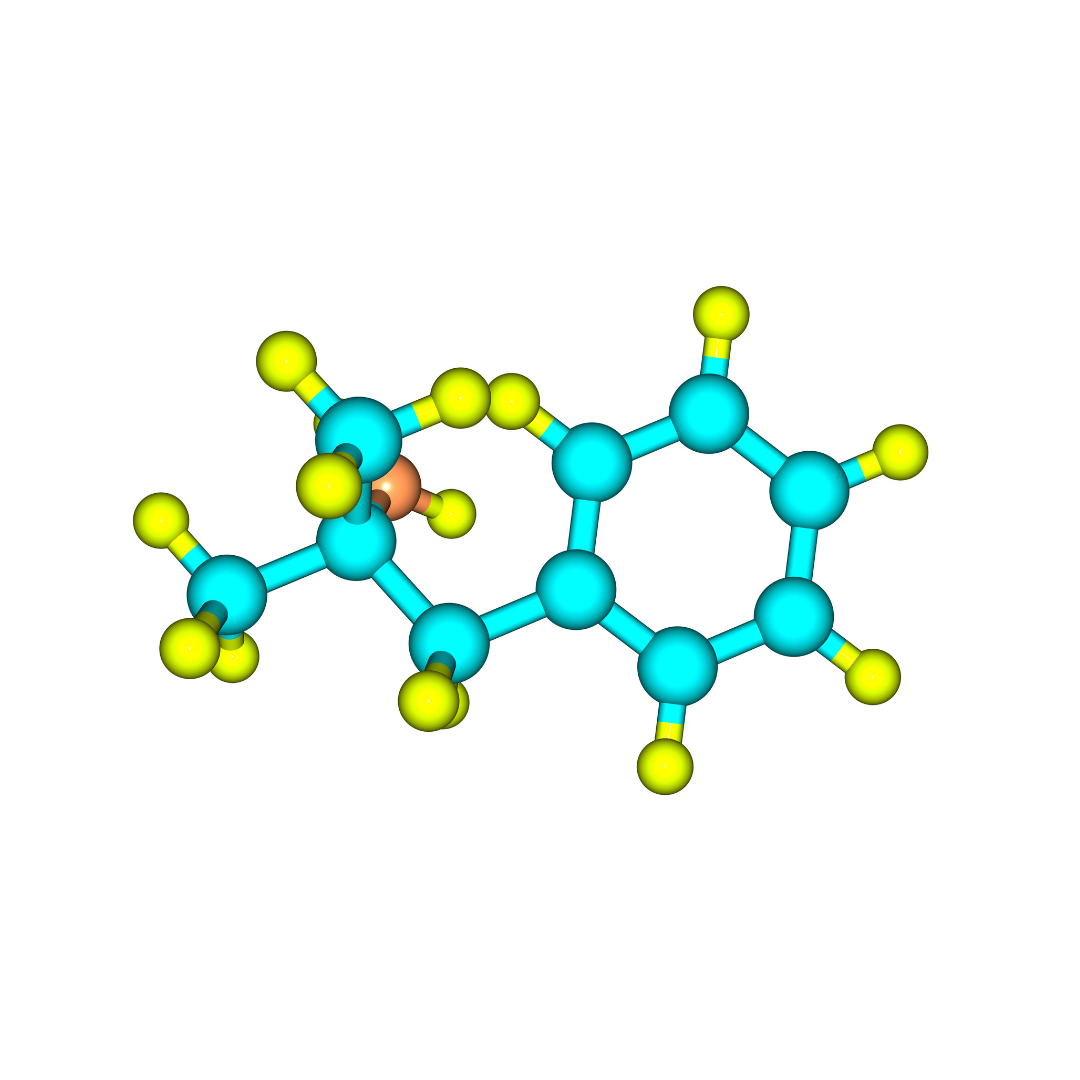
Why Phentermine?
- Increased metabolism. Phentermine not only lowers appetite but also increases the amount of energy we burn each day. The medication is a non-amphetamine stimulant. Speed of weight loss depends not only on calorie intake but also on calories burned. An increase calorie burn of 10% can make a significant difference in weight loss.
- Long duration of action. Phentermine has a long half-life, so it only needs to be taken once daily in most cases. The onset of action is gradual, and it wears off quite slowly. Taking phentermine at noon provides appetite control into the early evening, the most difficult time for most patients.
- Safety. There are few medications that have as long a track record as phentermine. It is well tolerated in the vast majority of patients for both short and long-term use. Millions of prescriptions have been written since its approval in 1959. It has a low risk of dependency.
- Cost considerations. Phentermine is one of the least expensive medications. It is more favorable compared to some of the new brand-name medications.
The choice of weight loss medications is a complex one. Each patient’s medical situation is different. The response to previous medications will help a clinician determine the best choice of anti-obesity medication for their weight loss program.
This is How You Lose the Weight, Once and For All
If you’re ready to say goodbye to quick fixes that never last? And you’re serious about losing the weight for good? We’re the experts you can trust to guide you through a weight loss program that will not only take the weight off but keep it off.
Schedule a consultation with us today.